In a quiet corner of East Melbourne sits the Bionics Institute and a world-changing team of researchers, clinicians and engineers. Together they explore the frontiers of using technology to create bionic solutions to debilitating diseases.
Today CEO Damon O'Sullivan sat down with Robert Klupacs, their CEO, to talk through some of the incredible work being done, and get his reflections on driving innovation and invention.

In conversation
Robert Klupacs, CEO at Bionics Institute
Damon O'Sullivan, CEO at Today


Can we start with a lay-persons definition of bionics?
My generation grew up watching the Steve Majors as “Six Million Dollar Man” – Better, stronger, faster… It’s not quite that.Simply put, bionics is the interface of biology and electronics, to bring about a positive impact on our health.
And how did the Bionics Institute come about?
It was created by Professor Graeme Clark in 1984. He was a university professor and ENT surgeon, with a passion to develop devices to overcome deafness. He is the original inventor and leader of the multi-disciplinary team that developed the cochlear implant. In order to fund his early research activities, Graeme was able to obtain the backing of a diverse group of benefactors which enabled him to establish his own not-for-profit institute to fund further research.
While the Bionics Institute still continues to undertake world-leading research into hearing we’ve expanded upon Prof Clark’s legacy to build devices incorporating some of the technology within cochlear implants to address diseases such as epilepsy, Parkinson’s Disease, Stroke, Blindness and Inflammatory Bowel Disease.
The cochlear implant is about overcoming deafness by sending signals to the brain, but you are also doing work in early detection of hearing problems?
That’s correct. We have a very exciting device in development Eargenie™ which is a non-invasive system to enable objective measurement of a baby’s hearing capabilities by using light to measure brain activity in response to sound.
It’s understood by many that if you have an infant with hearing loss or deafness, the sooner you give the baby a hearing aid, or cochlear implant, the better chance they have of developing their language skills.
At the moment, the test for determining hearing impairment in babies is by the use of headphones that are fitted to the ears and the sound increased until the baby reacts, For example by crying. As you can imagine while paediatric audiologists are extremely gifted professionals this is a pretty gross measurement system.
So the idea of developing an objective measure to see whether the device has been fitted correctly has been something that’s been a major problem. The literature suggests that 30-40% of cochlear implants or hearing aids fitted in babies with hearing loss have been sub-optimally tuned.
With Eargenie™ we put a little cap on babies’ heads, containing light sources, and are able to monitor how much the brain is active in response to sound, providing a truly objective measure of hearing capability.

So is ‘smarter detection’ a growing area?
Yes. A great example is our work with Epilepsy.
People living with uncontrolled epilepsy (which is about one-third of epilepsy patients) face real challenges: they can’t drive, swim, shower or even pursue certain careers. Effectively they need to operate assuming a seizure can come at any moment.
While there are now many different drugs for doctors to try, because it is so difficult to objectively monitor how many seizures a patient is truly having, it is incredibly difficult for doctors to develop a personalised drug therapy approach for these patients that might work.
At present, the model is that the patient records seizure events and shows the doctor. Our collaborator Prof Mark Cook showed in a landmark study 7 years ago, that true number of seizures could be 50-100x those self-reported. – This is partly because there’s an amnesiac response to a seizure (where a patient has no memory of an event), meaning that seizures often go unnoticed.
Therefore doctors require accurate information. Specifically how many seizures are actually happening? And what happens to seizure number on different drugs.
The holy grail for doctors is to have real-time information for the patient. We’ve developed a device that can be implanted under the scalp, to collect brainwave activity, which can monitor seizures accurately twenty-four-seven over weeks, months or years. The device utilises technology from the cochlear implant. It also includes unique software algorithms to be able to obtain that data and then generate a report which will constantly be streamed to the patients iPhone, which can then be analysed by the doctor in real-time providing them with an objective method to identify effective drug treatments.
The device has the capability, with further development, to become a seizure prediction device.
It all came about due to the strong clinical involvement being linked with our skills in implant, engineering, data analysis, and algorithm development.
That’s incredible, so moving from detecting signals to predicting episodes. You’re also working on other products to intervene and treat diseases.?
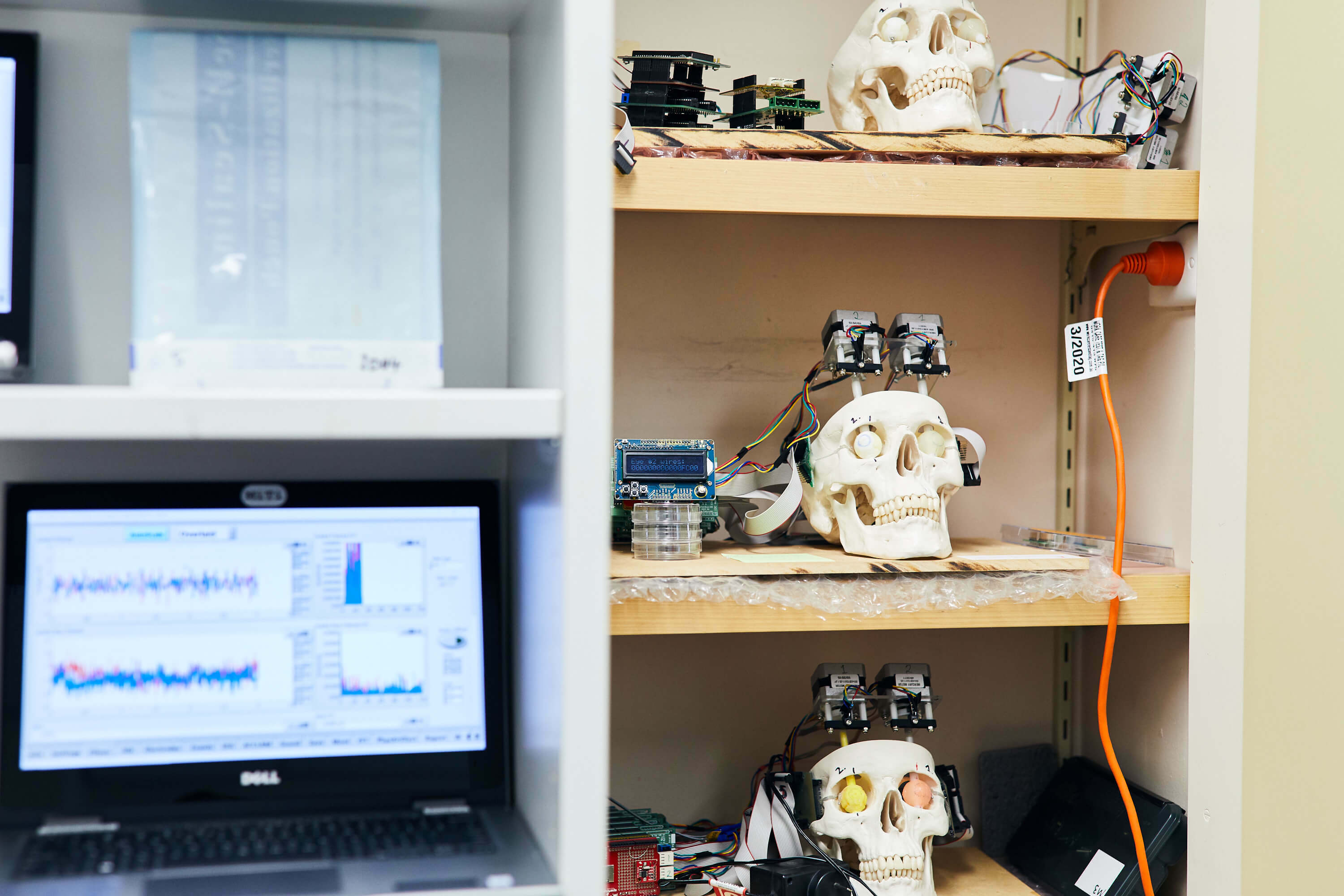
That’s correct. Through the fantastic relationship we have with the neurologists and neuro-surgeons at St.Vincent’s Hospital we are working to develop improved methods to treat the symptoms of Parkinson’s Disease, particularly tremors.
Over the last fifteen years, Deep Brain Stimulation (DBS) has been shown to be a very effective treatment. However, it still hasn’t achieved wide clinical usage as it some limitations. At the moment DBS can only be turned on or off by the patient meaning that the patient is over or under-stimulated which can cause unwanted side-effects. Additionally, because the surgical team needs patient feedback while the electrodes are inserted into the brain it currently requires the patient to remain awake. Therefore is also some very specific clinical talent involved. The electrodes need to reach and stimulate a part of the brain which is smaller in size than a grain of rice. If it misses the therapy won’t be effective.
We have found a unique electrical signal that accurately tells the surgeon whether the electrode has been placed in the right spot which appears to be present whether the patient is awake or asleep. We believe it will be game-changing as it will make it easier for surgeons to reach the right spot and hopefully enable them to perform the procedure with the patient asleep.
We are also excited because we believe this particular electrical signal can be used as a feedback loop to actually adjust the electrical pulse provided to the brain increasing or decreasing the stimulation level as required. This a holy grail for that field.
Another example which also uses nerve stimulation to achieve therapeutic benefit is a device we have developed in collaboration with the Florey Institute and clinicians at Austin Hospital. This time it's not to do with neurology in the brain, it's stimulation of a particular nerve that runs from the brain all the way to your gut (stomach) called the Vagus Nerve.
Crohn's disease and ulcerative colitis, which are known as Inflammatory Bowel Disease (IBD), are characterised by inflammation of the intestine and strongly nerve mediated. We have found that when we stimulate the Vagus Nerve as it interacts with the gut in a particular manner it has an anti-inflammatory effect. This has never been done before and, similar to the DBS technology, we've developed unique electrodes that can be implanted at a site in the Vagus Nerve, stimulating them accurately to overcome the inflammation and therefore treating this debilitating disease. Clinical trials should be starting late this year.
It’s genuinely exciting work, it feels like everything is moving quickly. In a field with so many possibilities, how do you choose? How do you decide what not to do?
It is hard. There’s a lot of things we’d like to do but can’t. We’re not going to cure cancer and we’ve decided not to work in the field of heart disease, at the moment. We also don’t work in the orthopaedic area.
Having said that because there is a common theme amongst our technology of stimulating or recording from nerves we do have the potential to work across many disease areas.
With us because we are so driven by addressing unmet clinical need a key driver for project selection is having a dedicated clinical champion in their speciality. For example, we formed a close collaboration with the retinal surgeons at the Centre for Eye Research Australia located at Eye and Ear Hospital to develop a “bionic eye”. As I mentioned before we are working closely with the neurologists and neurosurgeons at St.Vincents in the areas of Parkinson’s Disease and Epilepsy and gastroenterologists and gastric surgeons at Florey and Austin Hospital for our IBD work. We are also very lucky due to our long history in hearing research to have links with a number of Australia’s leading ENT surgeons.
And what do you do to keep people innovating? How do they invent the next thing?
You have to allow people to be creative and spend some time on areas of personal interest, not just the projects they are employed on.
Our staff are also encouraged to reach out to clinicians and say, okay, what’s your clinical problem? And what can I do? I’m an engineer/scientist, can I come up with a solution?
Once the connection is made while it doesn’t always lead to anything, in many cases we get this great alchemy.
I guess the other thing that assists in that regard comes back to the legacy we have built from the Graeme Clarke era. Graeme was passionate that you could only be successful if you embraced a multidisciplinary approach. That is core to what we do.
We have mathematicians, statisticians, software developers, software coders, data analysts, electrical engineers, mechanical engineers, physicists, patent attorneys, neuroscientists all interacting.
Plus we have built some fantastic relationships with specialist clinicians. It’s the combination of all those parts that leads to innovation.
The ‘fail fast’ approach, I feel like it’s something often repeated, but less often lived by. How do you deal with that?
I think the beauty of being a medical research institute per se, is that your idea is to come up with things that are novel which you hope might work but which might also fail. It’s to live on the creative edge.
What is “failure” anyway? Many times the concept is right but the prototype doesn’t quite work due to some technical glitches. This is actually a great opportunity because it forces you to re-assess, learn from what went wrong and make it right.
So it’s not a dead-end?
No. The challenge for us is only how much time we will spend on trying to get it right based on resources available to us in particular money. Having said that if people really want to do it, it’s amazing what they can do with sometimes with limited resources.
Any tips for leading people?
My job is simply to create the right environment so that the extraordinary people who work here can continue to create amazing things. That includes trying to inculcate a culture of pushing the envelope and accepting that although things don’t always work we can learn a huge amount from our “failures”.
The other thing I’ve learnt and it took me a long time to work out, particularly because I’ve worked in research my whole career, was that I kept thinking technology was the answer. Technology is obviously very important, but no product, particularly in the medical space, is “just” technology. Everything really comes from market-pull. That is are we solving a real problem? And if there is a problem, is it a meaningful problem, and will that solution actually make someone money? That’s why the Bionics Institute is such a dynamic place. The constant interaction with busy specialist clinicians keeps us extremely focused on the clinical problems that need to be solved.
How do you assess progress or momentum, when you’re inventing a device that’s never existed?
It’s always a process. The first thing that happens is a discussion that leads to a drawing on a paper.
The mere fact that you’ve moved to create a drawing, no matter how basic, means you’ve moved through the line. Then from that drawing, we try and work out how to physically make it. In almost every case you get these really rough looking prototypes. But over time, with iteration between scientists, engineers and clinicians it always amazes me how a working prototype emerges that can be assessed pre-clinically.
The hardest part is actually getting the ideas from discussions drawn down on a page. Once there is something tangible the process starts.
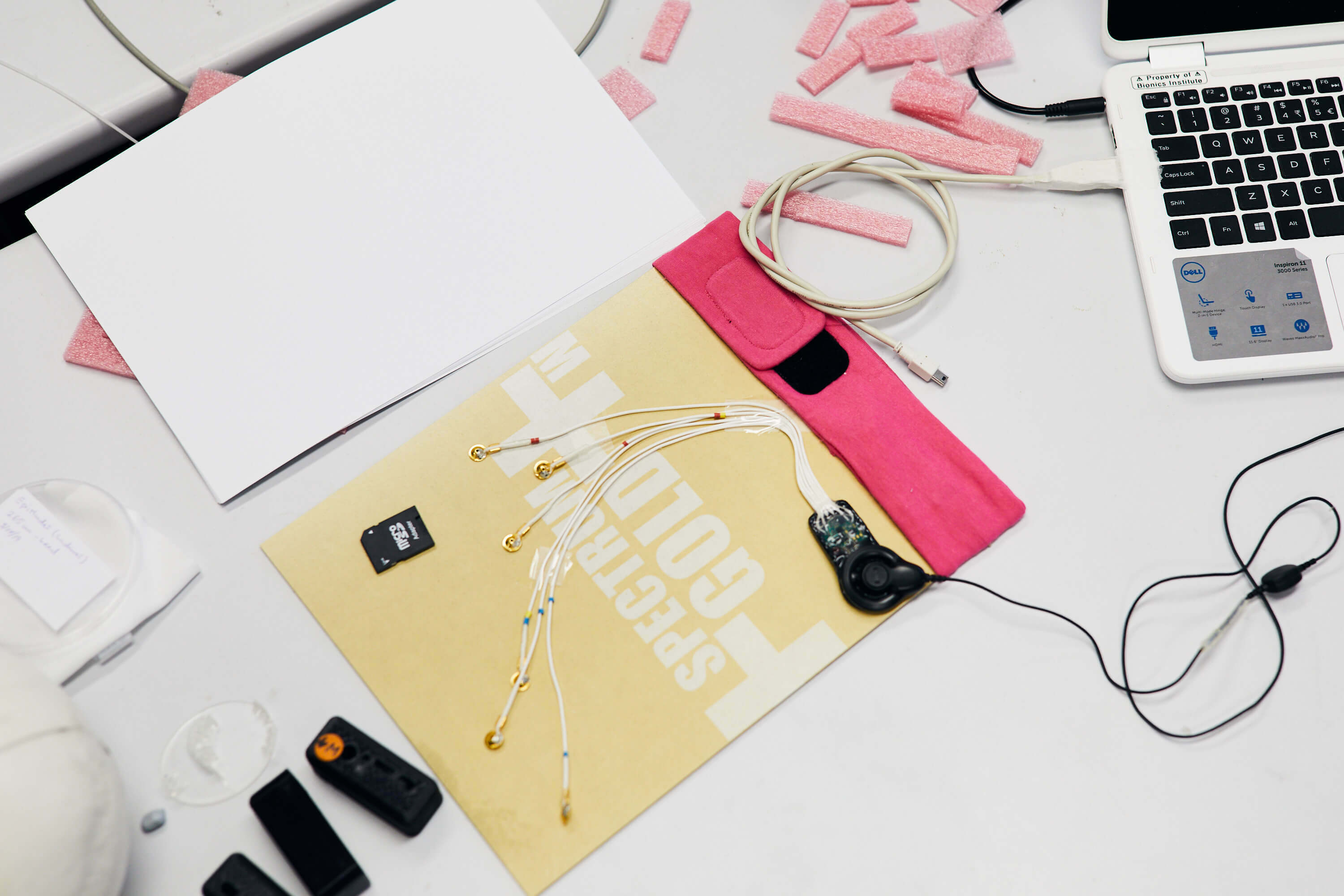
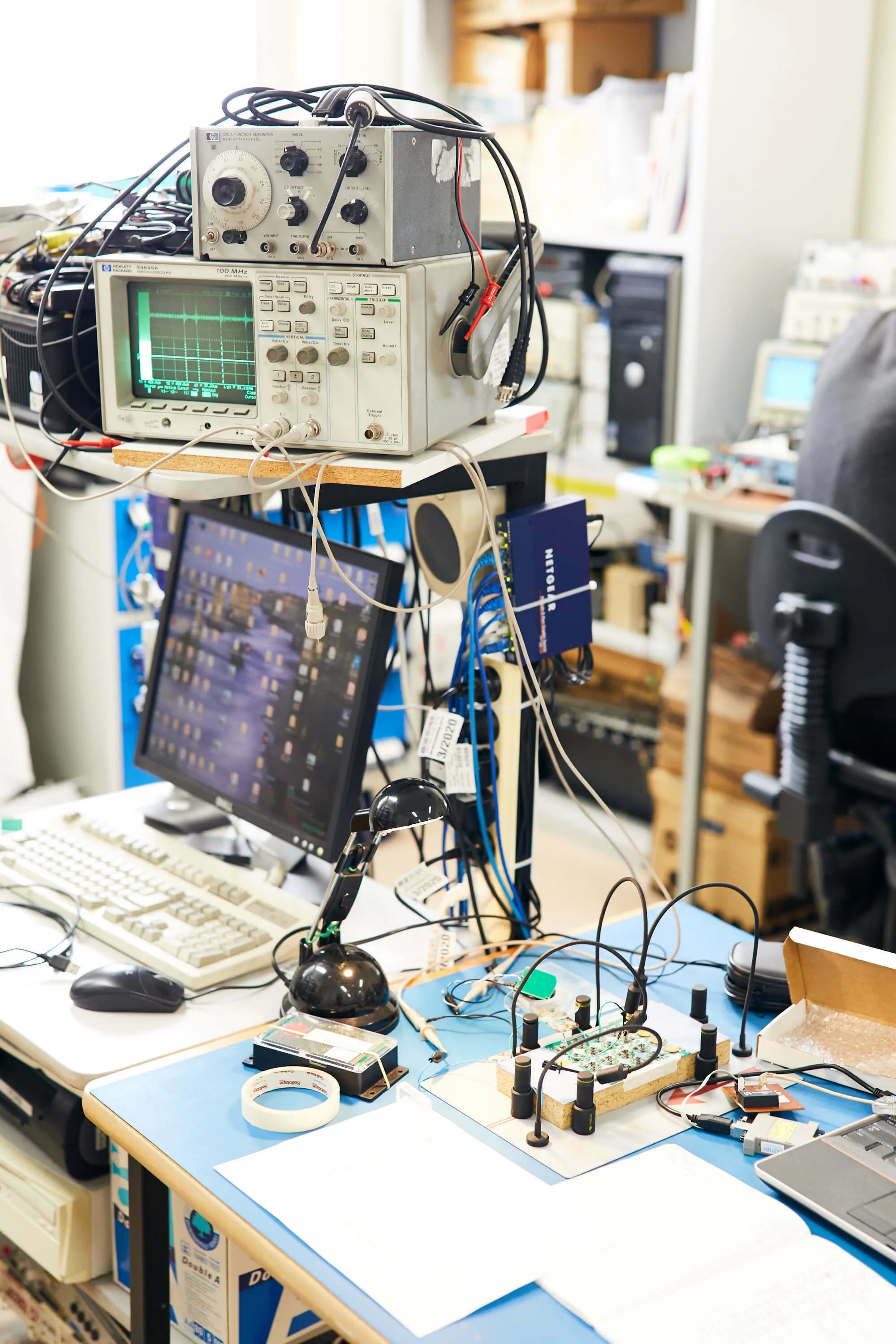
One thing that struck me seeing your labs is that sense of making, they almost feel like someone’s shed, building and tinkering.
Absolutely. I think you said it earlier, there’s a ‘fix it with fence-wire’ mentality.
We never want to lose that spirit of feeling like you’re working in your workshop or shed. By the same token, I say to my team, if you need me to get a ten thousand dollar piece of equipment so this work can be done in a day, rather than ten weeks, talk to me. I love that they strive to have the badge of honour that they can come up with stuff with limited resources, but we are also always pushing.
There’s the narrative that Australian’s are great inventors, but we can’t make it here. Does that ring true for bionics?
I actually don’t think that it does.
We don’t really make the big stuff anymore. We don’t build cars. We don’t build bulky stuff. But underneath that, Australia does manufacture quite a lot of small volume, high-value equipment, it’s just that not many people in this country seem to be aware of that.
Where I think Australia, and by extension us at the Bionics Institute, are going to excel is exactly in that space: small volume, high quality, and high-value medical devices. For example, the epilepsy device is a great example. Obviously, the success of Cochlear should make people realise it can be done.
Cochlear in Sydney manufacture forty to fifty thousand cochlear implant units a year. The numbers don’t sound high, right? Yet it generates approximately a billion dollars worth of sales per year worldwide.
I’ve heard quite a few people say China’s going to beat you. Well China’s great on high volume goods, but at present not so good in the areas of low-volume, high quality, high-value goods, That can and should be Australia’s niche.
Are you optimistic about the future?
Absolutely.
There’s a lot of incredibly intelligent and gifted people here and across Australia.
There are pockets of infrastructure. Our challenge, which I know we can meet, is to bring this together better and more efficiently. And then we’ve got to just believe in ourselves.
Australians, as you know, tend to talk ourselves down. And that’s what I’m trying to change here. Remind people that we are good, I’d say we’re up there in the top two or three in the world in the medical bionics space, and there is no reason we can’t be successful.
Want to support more of this incredible work? You should make a donation to the Bionics Institute.
